Spontaneous labour and birth is the dance of love and surrender between mother and baby with Oxytocin, the hormone of love and bonding, the orchestrator of all.
Modern medicine has led to increasing interventions that attempt to replicate this intricate process often before the mothers body and baby are ready. Though there are certainly times when induction of labour is indeed recommended, reasons for inducing and the frequency at which it is recommended have changed dramatically over time that do not always support better outcomes. The process of induction of labour and often its ensuing cascade of interventions is the bringing on of labour in a woman who was not previously showing any signs of labour, such as uterine contractions. Induction of labour ignores the holistic and complex whole being experience of birth with negative effects that can last a lifetime. Medical induction focusses on only the physical aspect of labour, the uterus and the cervix rather than labour and birth as all encompassing.
Induction of labour (I.O.L) has significantly concerning figures globally with 25% of all deliveries in developed countries and similar rates in non-developed countries. Guidelines, recommendations and hospital/practitioner practices vary widely between individual countries. Birth is cultural and where one establishment may recommend an I.O.L at 41 weeks, another may consider 42 weeks and beyond a perfectly reasonable and safe gestation with no need to interfere. Fear based care has become the norm within Western culture where the need to control, measure and manage labour and birth within a one size fits all approach (hospital policies) is standard practice.
Intending to ‘bring on’ labour and birth has been the focus for many pregnant women world-wide for thousands of years therefore not a new concept by any means but certainly one that has evolved to utilising technology, techniques and drugs that all have their risks and possible benefits. Women who request induction with no medical reason need to be well informed of the cascade of interventions she is essentially signing up for. It is important the woman utilises the B.R.A.I.N technique before commencing any form of induction.
These are essential questions to ask herself and her care provider before her true consent can be given.
Benefits. What are the benefits of induction and/or the method offered?
Risks. What are the risks of the induction and/or methods offered?
Alternatives. What are the alternatives to the induction methods offered?
Instincts. What are my instincts telling me?
Nothing. What if we do nothing?
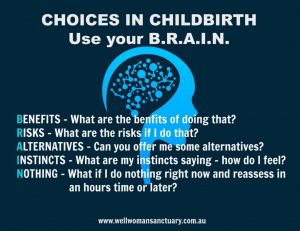
It is also of utmost value and responsibility of the woman to do her own research and ask any of her own questions of her provider she may have before consenting.
I.O.L can be lifesaving in situations that require the birth of the baby efficiently and quickly. Often these reasons are complex however the goal is always to reduce the risk of harm to mother and baby. However, modern times have shown that interfering with natures dance can cause more harm than good when applied to mothers and babies that are not at immediate risk. Examples where induction is not for reasons of immediate risk; postdates, mothers request, convenience to Doctor/Midwife/Hospital and suspected large baby. Reasons of clear medical indication for I.O.L include; HELLP syndrome, Preeclampsia, IUGR, infection, vaginal bleeding, still birth, uncontrolled gestational diabetes and high blood pressure.
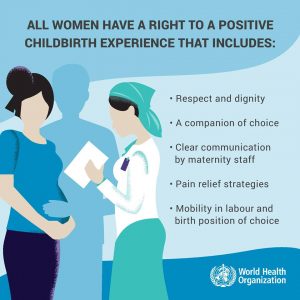
Individual circumstances and the woman’s right to bodily autonomy are paramount in deciding the best course of action with guidelines being just that, a guide, not a binding document that should be viewed or adhered to with disregard to the rights and decisions of the mother and her partner. Efficiency, productivity and being on time are not the values of most birthing families though certainly are for most hospitals and hospital care providers. The World Health Organization has provided guidelines for I.O.L that is evidence-based and recommended that all birth professionals adhere to first and foremost.
• Induction of labour should be performed only when there is clear medical indication for it and the expected benefits outweigh its potential harms.
• In applying the recommendations, considerations must be given to the actual condition, wishes and preferences of each woman, with emphasis being placed on cervical status, the specific method of induction of labour and associated conditions such as parity and rupture of membranes.
• Induction of labour should be performed with caution since the procedure carries the risk of uterine hyper-stimulation and rupture and foetal distress.
• Wherever induction is carried out, facilities should be available for assessing maternal and foetal wellbeing.
• Women receiving syntocinon, misoprostil or other prostaglandis should never be unattended
• Failed induction of labour does not necessarily indicate caesarean section.
• Wherever possible, induction of labour should be carried out in facilities where caesarean section can be performed.
Along with evidence based improved maternal outcomes these guidelines support the notion that normal physiological birth should be promoted, encouraged and supported unless there is clear medical indication to the contrary however the woman’s informed consent is imperative above all else. Induction is not risk free, often very painful, restrictive and can lead to a cascade of interventions. Birth mapping is a very useful, educative tool to create an informed birth plan that addresses each scenario the woman will face particularly in an induction.
A lot of women are unaware of the incredible abilities of their bodies, with great distrust in their body to even commence labour without artificial assistance. This lack of confidence can largely be attributed to birth becoming a big business in Western cultures whereby obstetricians are viewed as the Rolls Royce of maternity care, though frequently paternalistic in their treatment of birthing women and making a hefty financial gain in exchange for managing care despite there being no real evidence of its benefits in low risk pregnancies. Midwives are trained in physiological birth; obstetricians are trained in obstetric surgery and often have never attended a physiological birth.
So what is a physiological birth?
Physiological birth commences with changes in the woman’s cervix becoming softer, opening, thinning and moving forward to which begins to happen weeks prior to labour initiating. The baby influences when the naturally occurring hormones and processes are triggered therefore labour is a largely unpredictable occurrence that can start suddenly or gradually. Tightening’s of the uterine muscles (contractions) draw the cervix up causing effacement and dilation as the baby’s head/bottom gently presses down on the cervix. Oxytocin and endorphins, a naturally occurring hormone cocktail designed to relieve pain and create feelings of euphoria work together to not only bring baby earthside but to support the mother through the intensity of birth.
All induction methods require a favourable cervix, that is, a soft stretchy cervix. Using the Bishop score the woman’s cervix is assessed prior to any induction for her eligibility. Effacement, dilation, position and station must be determined before any means of induction commence.
There are several ways care providers attempt to initiate labour via chemical or mechanical means. All induction practices and drugs used carry their own inherent but very real risks. Despite this common knowledge among care providers, such practices and drugs are widely overused and recommended to birthing women. The cascade of interventions a woman experiences when accepting even the mildest form of induction often leads to risks and unfavourable outcomes. True consent involves sharing evidence based information that is true, current and correct rather than bias, negative language designed to ensure compliance through fear.
Low risk birth should not be feared, rather revered and respected. The long term effects of inducing labour can often far outweigh the short term benefits if no real medical indication for such invasive and unpredictable interventions are required for the health and safety of mother and baby. Birth trauma is a very real and rampant phenomena that demands a change in maternity care. Change begins with education.
Methods of medical induction will be discussed below.
Stretch and Sweep
Often an uncomfortable experience whereby the care provider during a vaginal examination and only after thorough explanation of the augmentation (with clear consent given), will insert a gloved index finger into the favourable cervix and in a circular motion sweep/separate the amniotic sac between the cervix and baby’s head (or bottom).
This fairly quick procedure carries risk for infection, may bring on irregular contractions that can last for days thus interfering with rest, cause light bleeding and sometimes be quite painful.
It is thought that the action of gentle massage and stretching of the cervix will release the hormone Prostaglandin and commence labour ‘naturally’ however more often than not will not as the mother and baby are not ready. Though this procedure uses no drugs, it is still considered an intervention and is not ‘natural’ despite most care givers recommending it as such.
Risks involved include prodromal labour, PROM, bleeding, pain and the psychological effects of creating a mistrust in her own body’s ability to go into labour.
Benefits are that it is helpful in reducing the number of women going over 42 weeks and can be repeated after 48 hours if no labour response evident.
Synthetic Prostaglandin
A pessary, suppository, tape or gel is inserted high in the vagina or rectum or a tablet can be taken orally, causing contractions to commence. Contractions can be quick to start and intense to which may cause fetal distress. Such contractions are not always indicative of a dilating cervix (progress) though and may also result in unpleasant effects.
Due to the effects of this medication it is not recommended for women with epilepsy, ruptured membranes, polyhydramnios, previous major abdominal surgery including caesareans, unexplained bleeding in pregnancy, multiple pregnancy or if the baby is not engaged.
By introducing synthetic Prostaglandin it is thought to soften and open the cervix and trigger labour to commence, yet it may not be enough to kickstart contractions. The woman will generally be required to remain in hospital for this as repeat doses are usually given every 6-8 hours in order to encourage this. Previous caesareans are contraindicated with an induction of vaginal birth using Prostaglandin.
Due to the effects of this medication it is not recommended for women with epilepsy, ruptured membranes, polyhydramnios, previous major abdominal surgery including caesareans, unexplained bleeding in pregnancy, multiple pregnancy or if the baby is not engaged.
Risks include over stimulation of the uterus, nausea, vomiting, diarrhea, flushing, shortness of breath, hypotension, pyrexia, uterine hyperstimulation, vaginal heat and tenderness, strong pain, baby HR abnormalities and rarely, uterine rupture.
Benefits include increased likelihood of vaginal birth within 24 hours.

Foleys/Balloon Catheter
A small catheter tube is inserted into the woman’s cervix during a V.E (after consent given) and saline is then introduced via syringe to inflate a small balloon between the baby’s head and the cervix. The tube is then taped to the woman’s inner thigh for up to 24hrs unless it falls out prior. The balloon adds pressure to the cervix similar to that of the baby’s head or bottom, mechanically opening the cervix rather than chemically.
Benefits include reduced infection chances due to modern sterilization practices, lesser side effects compared to prostaglandin, may start spontaneous labour, less likely caesarean rates and neonatal admissions.
Side effects are minimal, yet labour is often longer than spontaneous labour. There is still risk for infection, vaginal bleeding, PROM and can be uncomfortable.
Artificial Rupture of Membranes
An A.R.O.M involves mechanically breaking the amniotic sac, releasing the amniotic fluid resulting in the further descent of the baby’s head which then increases pressure on the cervix. This triggers hormone prostaglandin release and labour. When induced the important steps of preparation of the body are skipped and therefore the baby and woman’s body have essentially not triggered release of prostaglandin or oxytocin, instead is being forced to respond to the chemicals of labour rather than the physiological processes of spontaneous labour.
Endorphins are the bodys natural response to assist in pain management during birth, however with the contractions coming much quicker and stronger due to the result of induction methods it becomes incredibly difficult for the woman to not find herself in fear and panic. Fear creates tension, tension creates pain. Adrenaline and catecholamines are the arch enemies for a relaxed, open birth. These hormones are designed to assist in situations of fight or flight, not a safe supported environment conducive to a beautiful, transformative surrender to physiological birth.
Benefits include shortened labour, descent of baby, liquor check possible.
Risks include cord prolapse (obstetric emergency), cord compression, infection and increased risk of caesarean.
Synthetic Oxytocin (Syntocinon/Pitocin)
Administration of synthetic oxytocin requires the woman to be hooked up to an automatic pump via an I.V to which gradual doses are delivered to her blood stream. This intervention can be restrictive as the drug is a dangerous drug that can have severe impacts on mother and/or baby. Contractions are frequently leaving women unable to cope as they would in a spontaneous labour with surges on top of each other and intense. With continuous flow of the drug, baby does not cope so well either as the compressions caused by contractions are too frequent to give baby adequate time to recover from reduced blood flow. The drug does not cross the blood brain barrier therefore the woman does not receive the potent cocktail of endorphins that assist in her pain relief and rest.
Benefits include commencing labour when medically indicated, increasing contraction effectiveness and managing post-partum haemorrhage during third stage of labour.
Risks include uterine rupture, cardiac abnormalities, dizziness, skin rashes, hyper stimulation of uterus, distressed baby, suffocation of baby, death of baby, headache, nausea and postpartum depression.
Evidently, all induction methods call for in depth consideration before committing to the induction of labour. Each has its risks and possible benefits however the greatest concern to consider before consenting to any methods is the cascade of interventions that more often than not, lead to poor outcomes as a result. Each birth is unique. A woman holds so much power and wisdom in her ability to birth her baby the way she chooses to. We want to ensure mothers have bodily autonomy and understand the risks should she choose to consent before fully understanding them. We want our mothers to trust their bodies, their intuition and the process. Natural labour and birth is much more than the medical event it has evolved to be.

Birth is magic.
Birth is power.
Birth is transformative.
My name is Kristy Day and I am a Doula based in Dawesville, Western Australia who has trained with the Doula Training Academy. If you would like to talk more about your birthing options, please contact me:
Business Name: Queen Bee Birth
Business Website: www.queenbeebirth.com.au
Business Phone: 0403 880 204
Facebook: www.facebook.com/queenbeeperthdoula/
Instagram: https://www.instagram.com/queenbeebirth_doula/

