The hot topic landing on our lips recently is “vaginal seeding.”
You may have heard of it recently in the last few years or it may be a new subject. Firstly, vaginal seeding is a term used to describe the use of a gauze swab to transfer maternal vaginal fluid, and hence vaginal microbiota, on to an infant born by Caesarean section.
About an hour before the C-section, your healthcare provider takes a piece of sterile cotton (gauze) and places it inside your vagina. During this time, fluid collects on the gauze. Before the C-section begins, your healthcare provider removes the gauze and puts it in a sterile container. This container protects the vaginal fluids and microbes during C-section surgery.
Right after delivering the baby, your healthcare provider performs the vaginal seeding by taking the swab and then wiping them onto the baby’s face, mouth, eyes and skin.

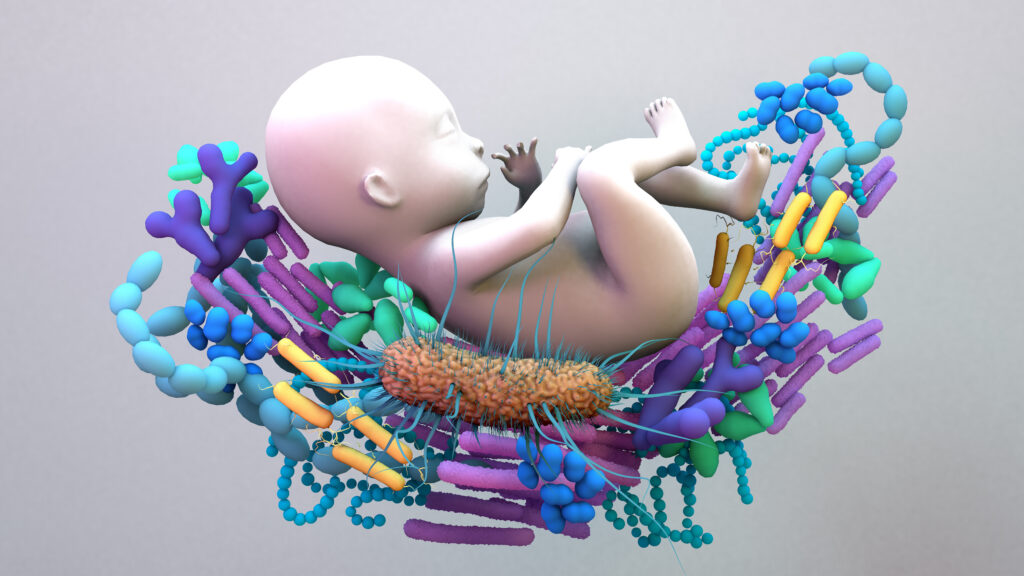
Microbiota is the community of microbes that colonizes our bodies, outnumbering our own cells 10 to 1. This complex microbial community varies from one part of the body to another, and from one person to another. A baby who is born by caesarean has not been in contact with this because they have not been birthed through the birth canal. Just like anything birth related you would be wanting to weigh up the risk vs the benefits for YOU. With this particular procedure there isn’t any sufficient amount studies yet to really support or refute it. What we do know is the babies born via c section have higher rates of asthma, obesity, diabetes in later life because they are not exposed to that microbiome.
A woman named Maria Gloria back in 2015 explored this and discovered that birth by caesarean section significantly altered the newborn child’s microbiome compared to that of a baby birthed via the birth canal. The evidence suggests that applying microbes from the mother’s vaginal canal to the baby after caesarean section may aid in the partial restoration of the infant’s natural gut microbiome with an increased likelihood of pathogenic infection to the child via vertical transmission.
But, in saying this there is no extra risk by doing this via vaginal seeding than by a vaginal birth. There are risks associated with birthing a baby via the birth canal also that can have transmission from mother to baby such as strep B, HIV, Chlamydia, and hepatitis C just to name a few. The risks of those transmissible diseases and infections are very low and you should first note the mother’s health and status of these infections.
Also, the incidence of neonatal Group B streptococcus infection ranges from 0.2/1,000 live births to 1.71/1,000 live births.
Risk factors for early onset Group B streptococcus infection of the newborn include maternal colonization during the pregnancy, previous infant with Group B streptococcus infection, preterm birth, prolonged rupture of the membranes and maternal fever during labour (Ohlsson & Shah 2009). There is low-level evidence that Group B streptococcus colonization in a previous pregnancy may be a risk factor for recolonization in a subsequent pregnancy (Cheng et al 2008; Turrentine & Ramirez; 2008; Tam et al 2012) but this association was not found in all studies (Weintraub et al 2011). HIV infection does not appear to increase the risk of colonization (Shah et al 2011).

Infants delivered vaginally are exposed to beneficial microorganisms known as microbiota when they travel down the birth canal. Infants are exposed to critical bacteria via vaginal birth, such as Lactobacillus, prevotelle, Bacteroides, Escherichia/Shigella, and Bifidobacterium.
Bifidobacterium is a key bacterium in the nourishment of the infants, development of immunity, and maturation of the intestinal tissue. The expectation is that this may boost their gut bacteria and lessen the danger of health issues normally associated with caesarean infants. It contributes to the seeding of the infant’s gut.
In the event of a baby being born via c section they come in contact with skin microbes, such as Staphylococcus, Streptococcus, Veillonella, and Corynebacterium. A very different set of species. These differences, in turn, have been associated with increased risks of asthma, allergies, obesity and immune deficiencies. Thus, these differences appear more often in infants after a caesarean delivery than after a vaginal delivery, according to certain epidemiological data.

In 2016 a small study of 18 infants was published in the Journal Nature Medicine to look into the benefits of vaginal seeding. The microbiome of the four caesarean delivered infants receiving the microbial transfer was found to have a similar microbiome to the seven vaginally delivered infants. The results of the study suggest that vaginal seeding partially restores the neonatal microbiome.
Again, the research is limited to come to a clear conclusion. Each woman would have to consult their own health practitioner and support team to make a decision based on, when baby is born and weigh up the individual risks and benefits on vaginal seeding.
If you have your baby by C-section, there are other ways to give your baby healthy microbes, including breastfeeding and skin to skin contact.
My name is Carly Dart, and I am a student doula who is doing extensive training at the Doula Training Academy. If you would like more information about my doula services, please contact me:
Email:
[email protected]
Website:
www.carlydoula.wixsite.com/doula
Resources;
https://en.m.wikipedia.org/wiki/Vaginal_seeding
https://ranzcog.edu.au/news/vaginal-seeding
https://www.bmj.com/content/352/bmj.i227
https://my.clevelandclinic.org/health/treatments/22096-vaginal-seeding